The belly fat connection
Visceral fat—the fat around your organs—is metabolically active, releasing signals that worsen insulin resistance and raise inflammation. Reducing it improves fasting glucose, post‑meal control, and cardiovascular risk. The approach is not extreme; it’s consistent and sustainable.
Food first: build plates that work
- Protein anchors meals and preserves muscle during fat loss.
- Non‑starchy vegetables add volume, fiber, and micronutrients.
- Carbs are personalized; start with modest portions and test your response.
- Fats from olive oil, avocado, nuts, and eggs support satiety.
Sample day
- Breakfast: omelet with spinach and feta; coffee or tea without sugar
- Lunch: chicken salad with olive oil and lemon; olives or nuts
- Dinner: salmon with roasted vegetables and a side salad
- Snacks: Greek yogurt, cottage cheese, or cheese and cucumbers as needed
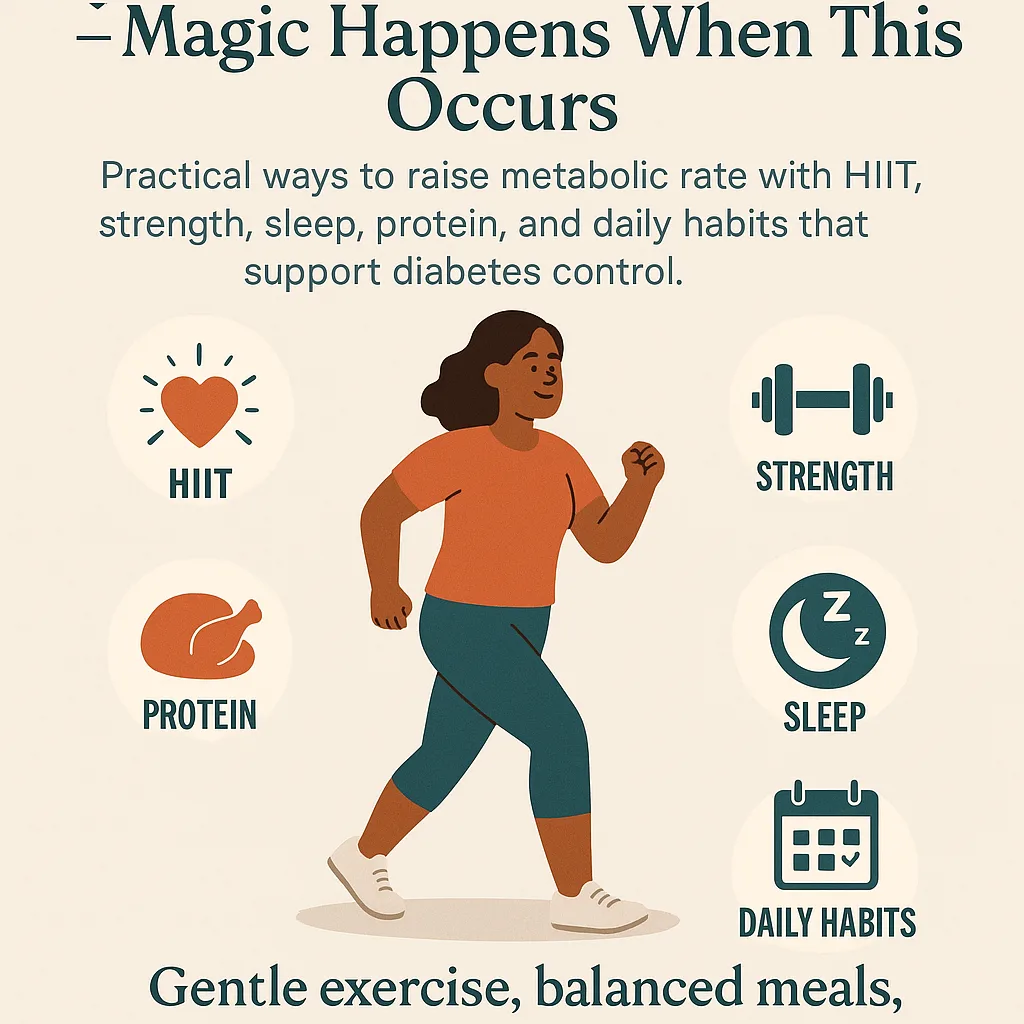
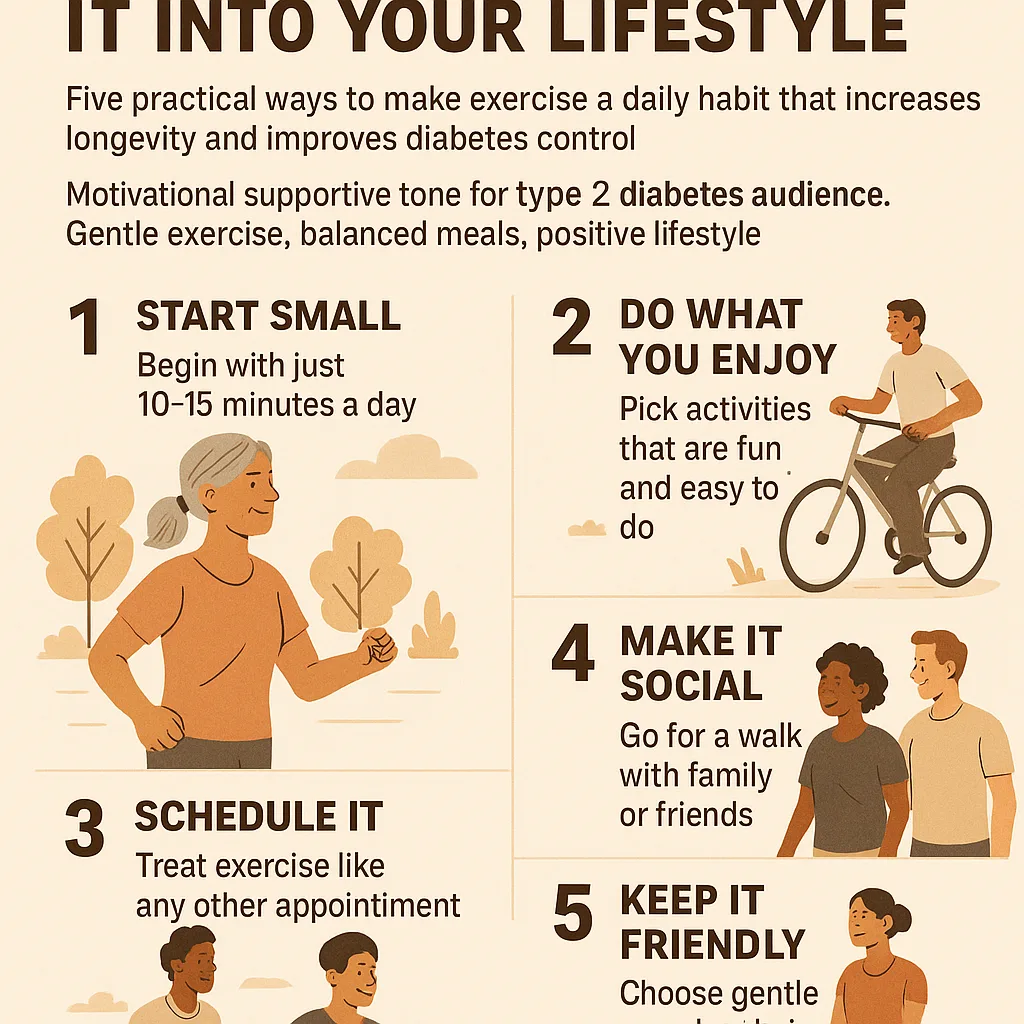
Movement: frequent and doable
- Walk 10–15 minutes after meals to blunt spikes.
- Strength train twice weekly to maintain or build muscle.
- Add gentle intervals to walks as fitness improves.
Sleep and stress: silent drivers
Short sleep and chronic stress push glucose higher and increase hunger. Protect 7–9 hours, reduce late caffeine and bright light, and use simple breathing or short walks to downshift.
Measure what matters
- Waist circumference alongside weight and how clothes fit
- Fasting and post‑meal glucose at 60–120 minutes
- Energy, cravings, and sleep quality
Troubleshooting
- Plateau? Recheck portions and liquid calories; increase protein and vegetables.
- Evening cravings? Front‑load protein earlier; add a warm, savory snack.
- Low energy? Improve sleep consistency; reduce interval volume for a week.
The payoff
As visceral fat decreases, insulin sensitivity improves. You’ll likely notice steadier mornings, fewer crashes, and easier portion control. The path is straightforward: protein‑forward meals, regular movement, quality sleep, and patient consistency.