Diabetes Complications: Part 2
Diabetes often develops quietly, and symptoms can be easy to dismiss. The sooner you recognize what’s happening, the sooner you can act to protect your eyes, kidneys, nerves, and heart. Tightening blood sugar control shifts the chemistry inside your body—reducing glycation, oxidative stress, and micro‑vascular damage—and opens the door to real‑world improvements.
What high glucose does inside the body
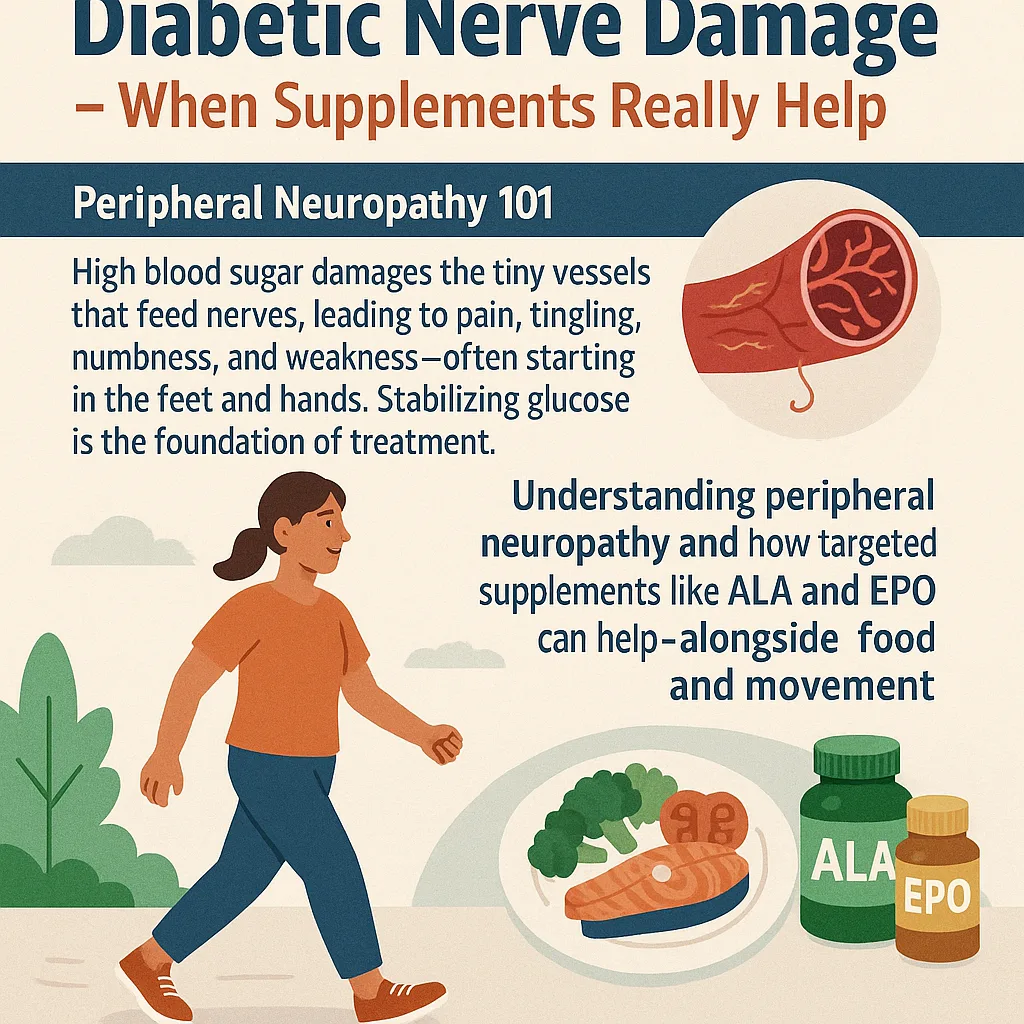
Chronically high glucose binds to proteins and fats, forming advanced glycation end products (AGEs) that stiffen tissues and impair function. The tiniest blood vessels suffer first, delivering less oxygen and nutrients to nerves and organs. Over time, this shows up as neuropathy, retinopathy, kidney strain, delayed wound healing, and cardiovascular risk.
Symptoms to take seriously
- Excessive thirst and frequent urination
- Fatigue, irritability, or brain fog
- Unintentional weight loss or stubborn weight gain
- Blurred vision, especially after meals
- Slow‑healing cuts, recurrent infections
- Tingling, numbness, burning, or pain in the feet and hands
These are prompts to test and treat, not wait and see.
Peripheral neuropathy in plain language
Nerves transmit sensation, control muscle movement, and help regulate automatic processes like digestion, sweating, and blood pressure. When glucose stays high, the nerves’ tiny support vessels fail to deliver enough oxygen and nutrients. As you normalize glucose day after day, the ongoing injury stops—and many symptoms ease as nerves recover.
A prevention and reversal plan you can start now
- Stabilize glucose.
- Build plates with protein first, non‑starchy vegetables second.
- Personalize carbs; fewer total carbs per meal usually means flatter curves.
- Move most days.
- A 10–15 minute walk after meals lessens spikes.
- Add two short strength sessions weekly to improve insulin sensitivity.
- Sleep 7–9 hours.
- Poor sleep drives glucose higher.
- Manage stress.
- Two minutes of slow breathing before meals helps digestion and glucose.
- Care for your feet.
- Daily checks, proper footwear, and early treatment of hot spots and cuts.
- Keep up with screening.
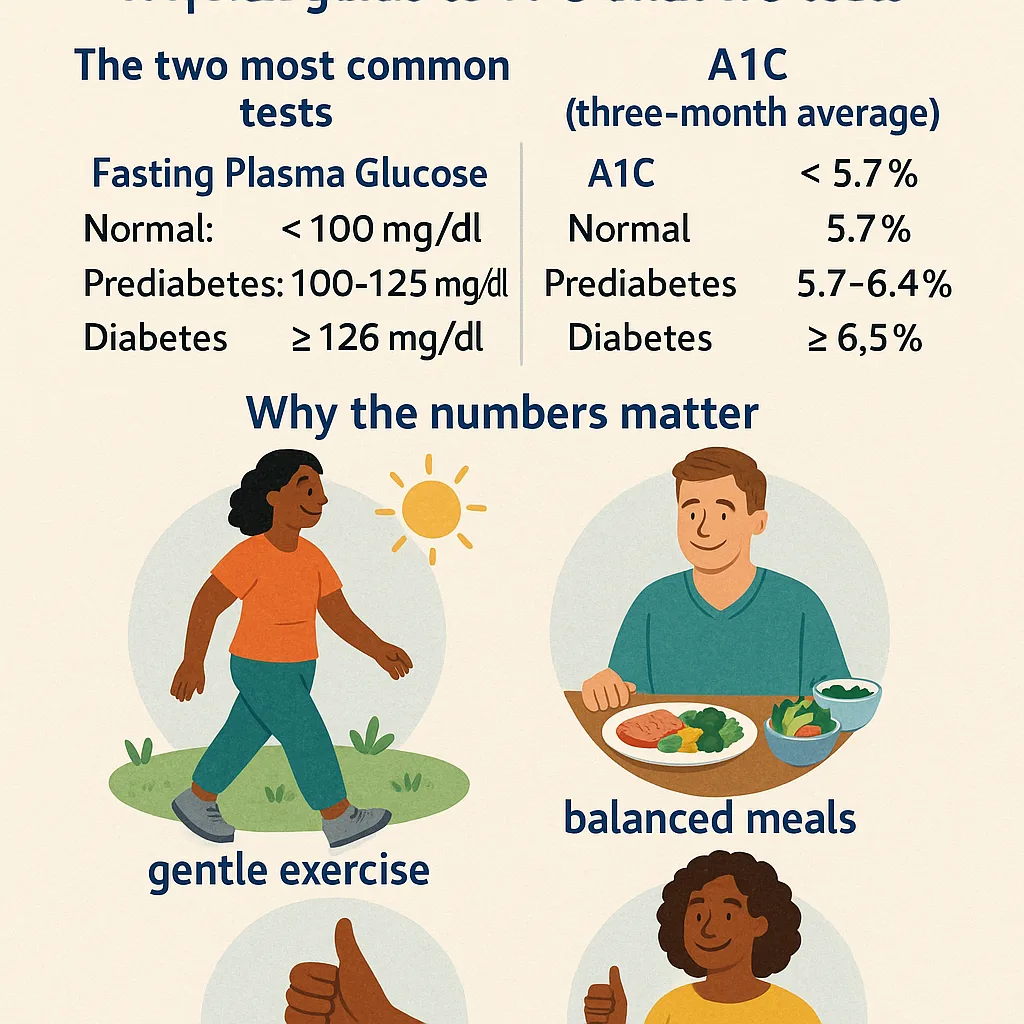
- A1C, lipids, kidney labs, and annual dilated eye exams.
When to call your clinician
New or worsening foot pain, sores that don’t heal, sudden vision changes, dizziness, or severe fatigue deserve prompt evaluation. Bring meter or CGM trends and a short food log to visits; data improves decisions. Never change prescriptions without medical guidance.
Real‑life reversal
Reversal means fewer symptoms, better function, and improved labs. People commonly report steadier energy, less burning or tingling in feet, improved balance, and calmer sleep once daily glucose stabilizes. Nutrient‑dense meals, modest weight loss where appropriate, and regular movement work together to reduce the metabolic burden on tissues.
Share what you learn
Because diabetes can be silent, awareness saves time and tissue. Share symptoms and prevention strategies with friends and family. Earlier action leads to better outcomes.